The natural consequences of growing old include slower wound healing and a brain that makes fewer new neurons because old tissues have less regenerative capacity. What has not been clear is why.
A trio of papers published online Sept. 6 in the journal Nature shows that old stem cells don’t simply wear out, they actively shut themselves down, probably as a defense against becoming cancerous from genetic defects that accumulate with age.
“The good news is that we can get older before we get cancer,” says Sean Morrison, director of the Center for Stem Cell Biology, and lead author on one of the three papers. “The bad news is that our tissues can’t repair themselves as well.”
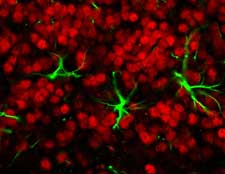
Though science long has known about the reduced regenerative capacity in aging tissues, the actual mechanisms only now are coming to light. What Morrison and his colleagues at Harvard University and the University of North Carolina (UNC) have found is that a gene called Ink4a actively interferes with the ability of stem cells to divide in several different types of tissue, including the brain, the pancreas and the blood-forming system of the bone marrow.
Under optimal circumstances stem cells are able to copy themselves and differentiate into other cells, thus replenishing their numbers and acting as a repair system for the body. The Ink4a gene appears to be widely active in locations where stem cells regenerate new tissues.
“The findings are remarkably consistent across the three papers,” says Norman Sharpless, an assistant professor of medicine and genetics at UNC, who studied the gene’s effect on insulin-producing beta cells of the pancreas. “Clearly there are tissues where this gene doesn’t play a role, but probably the effect is going to be much broader than in the few tissues we’ve identified.”
Morrison’s team also has shown that eliminating Ink4a partially restores the renewal of neural stem cells in some parts of the brain. “This is the first time that anyone has demonstrated it is possible to delete a single gene and rescue declines in either neurogenesis or stem cell function with age,” Morrison says.
Though mice with Ink4a deleted had more regenerative capacity in tissues like the brain and the pancreas as they aged, they started dying of a wide variety of cancers at one year of age. So it can’t really be said that losing the gene helped them live longer.
“If you had a drug that could inhibit Ink4a function, you’d potentially have a therapy against degenerative diseases,” Morrison says. “But you’d have to watch patients carefully for cancers. By the same token, drugs that mimic Ink4a function could be used to fight cancer.”
Ink4a was known to be a tumor suppressor gene that becomes more highly expressed with age, eventually triggering the cell to shut down replication. Sharpless was investigating cancer genes when he developed a mouse without Ink4a six years ago while working at Harvard, but he also became intrigued by its 10- to 100-fold increase in expression with age.
An important natural regulator of Ink4a is a gene called Bmi-1 that promotes stem cell maintenance and cell regeneration, but also can spur cancerous growth. Stem cells balance their levels of Bmi-1 and Ink4a to maintain themselves throughout adult life.
Morrison says these both are pieces of a finely calibrated system that allows needed cell replication to occur, but can shut it down when things get out of control. His team would like to find out more about the multiple factors that change Ink4a expression with age. He notes also that Ink4a doesn’t affect all of the cells of the nervous system in mice, just a subset of them.
The parallel papers grew out of a discussion between Morrison and colleagues at a conference. When they realized they all were working on the same idea, they decided to submit their papers to Nature together. David Scadden’s team at Harvard University explored the role of Ink4a in blood-forming stem cells.
Morrison’s work was supported by the National Institute on Aging and the National Institute of Neurological Disorders and Stroke—both part of the National Institutes of Health—and the Howard Hughes Medical Institute. His research team includes graduate students Anna Molofsky and Nancy Joseph, and research fellow Guy Slutsky.

